Extracellular vesicles as markers for prostate cancer
extracellular vesicles can be used as markers for prostate cancer. Most likely it's not going to be the vesicles themselves that carry important information, but their cargo[@ramirez-garrastacho2021]. The cargo may reflect the intracellular status and physiological state of their parental cells. The entire approach can also be included into the topic of liquid biopsy.
Gentle prostate massage can enrich the number of EV in urine, since it induces the secretion of prostatic fluid into the urethra, which is then mixed with urine. It is normally called DRE urine (Digital Rectal Examination).
The biggest challenge is that urine is a highly dynamic biofluid, and its contents depend on biorhythm, fitness, and diet[@ramirez-garrastacho2021]. Therefore the quantification of extracellular vesicles and different separation methods must be somehow linked to normalization factors. What is known is that prostate cancer-related proteins (and their mRNA), such as PAP, PSA, PSMA, PSCA, TGM4, TMPRSS2 are all found in urinary EVs.
Blood-derived EVs are more challenging to study, but they also show some correlation between prostate cancer and markers[@ramirez-garrastacho2021]. The question is, in that case, the mechanisms that govern the transfer of EVs (or of proteins such as PSA) from the urethra to the bloodstream. But this seems to be a second-order problem, with some partial anatomical explanations.
The general challenge for the use of EVs, as almost always, is related to the EV isolation and purification methods that can be used. This is not specific to the urine, blood, or the problem at hand, but pervasive to the entire research field.
One possible approach is to target CD9 and CD63, two tetraspanins normally found on exosomes, and use a second labeling agent that targets proteins specific to the cancer cells. This is something like what the ExoView device could, in principle, achieve. There's also a clear path forward for the EVQuant in case there is a double-labeling possible.
One possible path is to combine TR-FIA with europium labeling[@duijvesz2015a]. An essay similar to Elisa test with fluorescence is able to quantify the amount of CD9 and CD63 in urine samples from patients with and without prostate cancer.
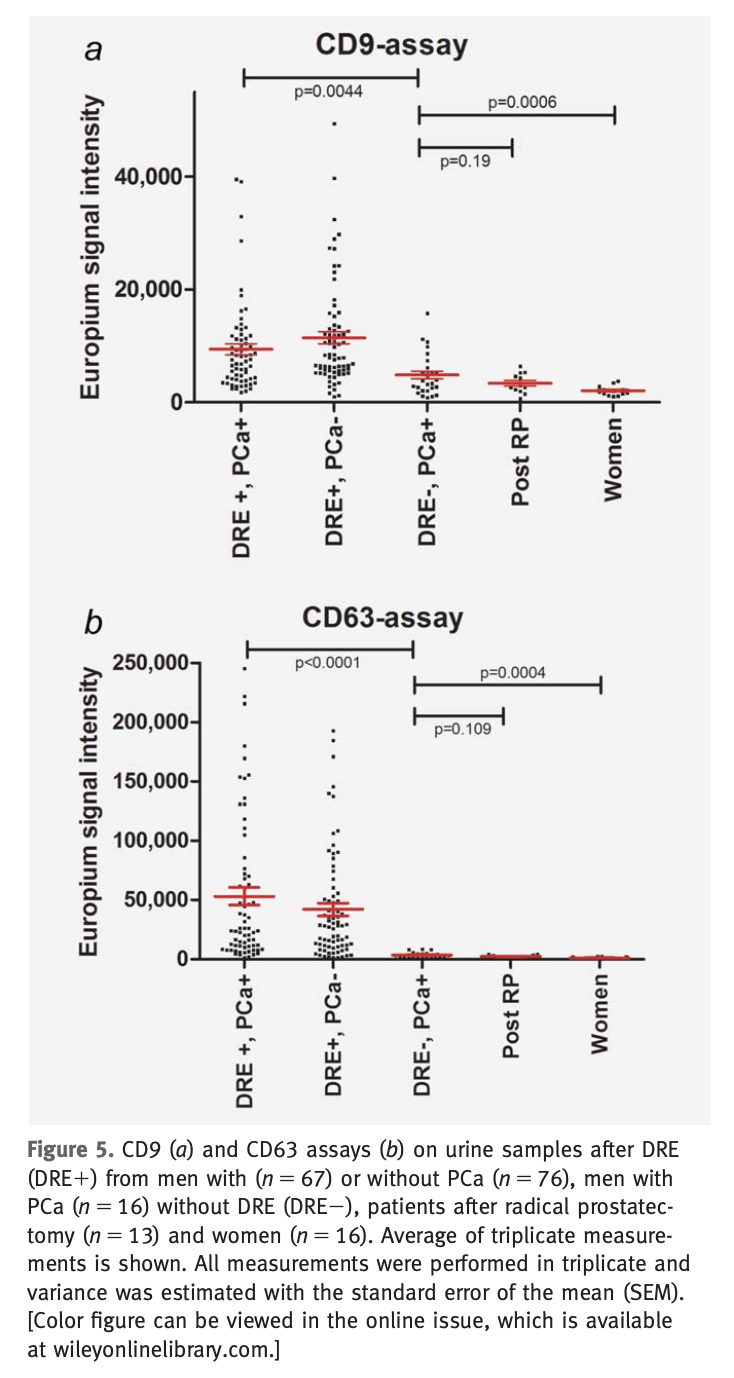
The overall idea is that quantifying the concentration of CD9 and CD63, it is possible to have a better diagnostic tool than by just looking at PSA levels.
However, care must be taken, since it is not the EVs themselves used as biomarkers, but either their cargo or composition. The advantage is that instead of doing a biopsy, one can perform a liquid biopsy and get the same proteins or markers. Most studies focus on the use of mRNA, miRNA, and proteins[@ramirez-garrastacho2021], but there is some insight showing that other molecules can be of interest, such as the lipid species or metabolites.
The bottom line is that multiplex biomarker assays perform better than single cancer biomarkers
Backlinks
These are the other notes that link to this one.
